AI and Machine Learning in Peer Review: Improving Efficiency and Reducing Bias

Artificial Intelligence (AI) and Machine Learning (ML) are revolutionizing various sectors, peer review in academic publishing is no exception. The integration of AI and ML into the peer review process promises to enhance efficiency, reduce bias, and ensure high-quality scholarly communication. This blog explores how AI and ML are transforming peer review, the potential benefits, and the challenges associated with their implementation.
Need for AI in Peer Review
The peer review process plays a key role in academic publication, to ensure the authenticity and quality of scholarly articles. However, this system is under significant strain due to the increasing volume of manuscript submissions. According to a study, manuscript submissions have been growing at an annual rate of 6.1% since 2013, leading to a substantial increase in the workload for peer reviewers. Traditional peer review is time-consuming, with estimates suggesting that over 15 million hours are spent annually on reviewing manuscripts often resubmitted to other journals after rejection [1].
AI and ML can alleviate some of these burdens by automating parts of the review process, thereby saving time and resources. These technologies can perform initial screenings, check for plagiarism, ensure adherence to formatting guidelines, and even assess the quality of a manuscript. Such automation can free up reviewers to focus on more complex and subjective aspects of the review process.
How AI and ML Enhance Peer Review
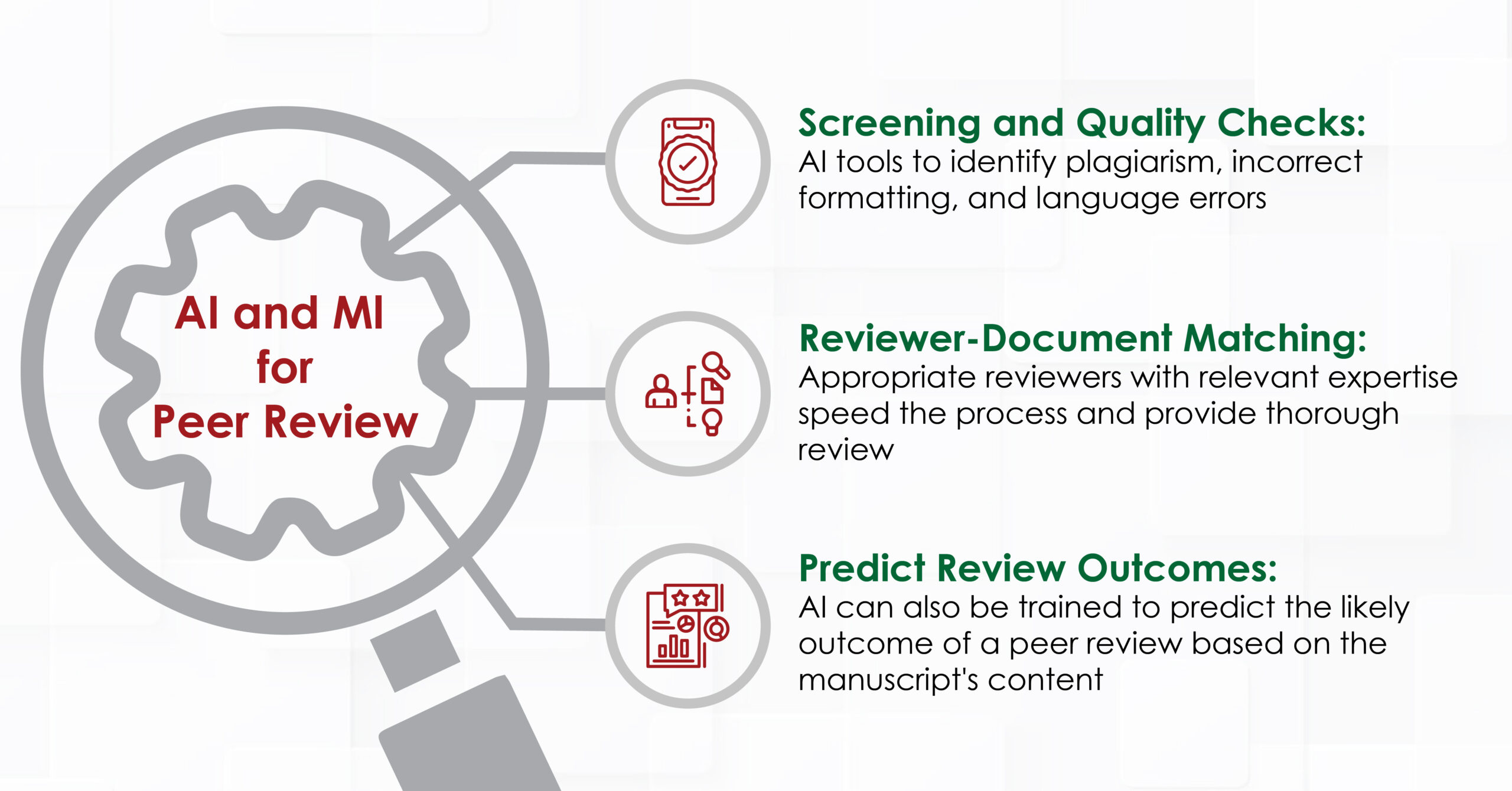
- Automated Screening and Quality Checks
AI tools can automate the initial screening of manuscripts. For example, software like Statcheck and Penelope.ai can verify the consistency of statistical reporting and check whether a manuscript meets a journal’s structural requirements. These tools can quickly identify common issues such as plagiarism, incorrect formatting, and language errors, which might otherwise delay the review process.
- Reviewer-Document Matching
Matching manuscripts with appropriate reviewers is another area where AI can make a significant impact. Traditional matching relies heavily on the expertise of journal editors, but AI can analyze the content of manuscripts and reviewer profiles to suggest the most suitable reviewers. This speeds up the process and ensures that the reviewer has the relevant expertise, potentially leading to more thorough and insightful reviews.
- Predicting Review Outcomes
AI can also be trained to predict the likely outcome of a peer review based on the manuscript’s content. A study demonstrated that a neural network trained on a large dataset of manuscripts and their corresponding reviews could predict review scores with a high degree of accuracy [1]. While AI cannot replace human judgment, it can assist editors in making preliminary decisions, such as identifying manuscripts that are likely to be rejected due to poor quality.
Reducing Bias in Peer Review
Bias in peer review is a well-documented issue. Reviewers may be influenced by factors such as the author’s institution, gender, or nationality, leading to unfair evaluations. AI and ML have the potential to mitigate these biases by providing objective assessments based on the content of the manuscript rather than the identity of the authors.
- Uncovering Hidden Biases
AI can be used to analyze patterns in review data to uncover biases. For instance, an AI tool trained on a large dataset of peer reviews might reveal that certain types of papers or authors are consistently rated lower than others, regardless of the content. This information can help journals to develop strategies to address these biases and ensure a fairer review process.
- Ethical Considerations
Despite the potential benefits, the use of AI in peer review raises ethical concerns. One major issue is the risk of perpetuating existing biases if the AI systems are trained on biased data. For example, if past reviews have favored certain demographics or institutions, the AI might learn to replicate these biases. Therefore, it is crucial to ensure that AI systems are trained on diverse and representative datasets.
Another concern is the opacity of AI decision-making. Authors and reviewers may be skeptical of AI-generated recommendations if they do not understand how these decisions are made. Ensuring transparency in AI algorithms and providing clear explanations of AI decisions can help build trust among stakeholders.
Case Studies and Current Implementations
Several initiatives are already leveraging AI to support peer review. For instance, the National Natural Science Foundation of China uses AI to assist in the grant review process, aiming to reduce bias and the workload on reviewers. Similarly, the Canadian Institutes of Health Research have implemented an online system to manage grant applications, which has been praised for its ability to reduce reviewer fatigue and improve transparency.
Another notable example is the use of AI in MOOCs (Massive Open Online Courses) to assess student essays. Automated Essay Scoring (AES) systems, used by platforms like EdX, MIT, and Harvard, have demonstrated the potential of AI to handle large volumes of written work, providing timely feedback and maintaining consistent evaluation standards.
Future Directions
The future of AI in peer review holds many possibilities. Ongoing research aims to enhance the capabilities of AI systems to handle more complex aspects of the review process, such as assessing the novelty and significance of research. Additionally, integrating AI with other technologies, such as blockchain, could further enhance transparency and accountability in peer review.
- Enhancing AI Capabilities
Future AI tools could be developed to provide more sophisticated analysis of manuscripts. For example, AI could be trained to evaluate the logical coherence of arguments, the robustness of methodologies, and the relevance of cited literature. This would require advances in natural language processing (NLP) and domain-specific training.
- Blockchain Integration
Integrating blockchain technology with AI could address some of the transparency issues associated with AI in peer review. Blockchain can provide a tamper-proof record of the review process, ensuring that all decisions and changes are documented and traceable. This could enhance the credibility and accountability of the peer review process.
Conclusion
AI and ML offer promising solutions to many of the challenges faced by the traditional peer review system. By automating routine tasks, improving the matching of reviewers and manuscripts, and providing objective assessments, AI can enhance the efficiency and fairness of peer review. However, it is essential to address the ethical concerns and ensure transparency in AI decision-making. As these technologies continue to evolve, they hold the potential to transform peer review, making it more efficient, equitable, and reliable.
The integration of AI and ML into peer review is not just a technological upgrade but a fundamental shift in how we approach scholarly communication. By harnessing the power of AI, we can build a more robust and inclusive peer review system that upholds the highest standards of academic integrity.
References
- Kousha K, Thelwall M. Artificial intelligence to support publishing and peer review: A summary and review. Learned Publishing. 2024 Jan;37(1):4-12.
- Checco A, Bracciale L, Loreti P, Pinfield S, Bianchi G. AI-assisted peer review. Humanities and Social Sciences Communications. 2021 Jan 25;8(1):1-1.
